Why Maternal Sepsis Is Such an Important Topic
April 23, 2018

It’s hard to imagine in this day and age that being pregnant and giving birth can result in life-threatening complications. However, this is the reality for over 60,000 women in the United States each year.1 While most women recover to their previous level of functioning, about 2,000 women die and some are left with lasting and life-changing issues.2 Not all complications related to pregnancy and childbirth are preventable, but some, like sepsis, may be avoided with increased sepsis awareness and quick recognition and treatment of infections.
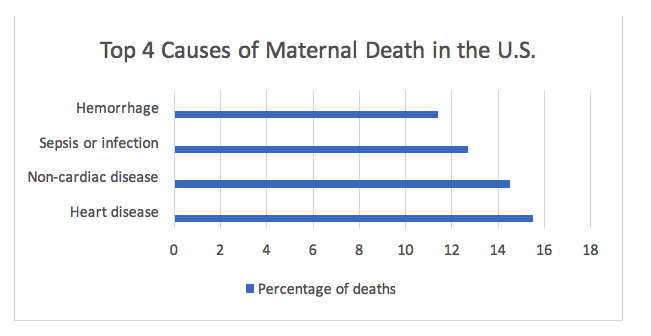
Sepsis is your body’s inflammatory reaction to an infection. It is responsible for 15% of all maternal deaths worldwide, and the Centers of Disease Control and Prevention (CDC) lists “infection or sepsis” as being responsible for 12.7% of pregnancy-related deaths in the U.S. This is the third most common cause, following heart disease (15.5%) and non-cardiovascular disease (14.5%).3
Risk factors for sepsis
Women who are pregnant could contract an infection that can lead to sepsis any time during their pregnancy and within the following weeks. Although maternal sepsis can strike anyone, these factors could increase the risk3,4:
- Miscarriage
- Abortion
- Invasive tests during pregnancy
- Cesarean section, which is a major abdominal surgical procedure
- Preterm delivery, having the baby before the due date
- Prolonged or obstructed labor
- Ruptured membranes, “water breaking” several hours before birth
- Postpartum hemorrhage, excessive bleeding after birth
- Stillbirth
- Retaining placenta after birth
- Multiple gestation (twins or more)
- Mastitis, infection in one or more breasts
- Chronic illnesses, like diabetes, which increase the risk of infection
Other terms for maternal sepsis
The term “maternal sepsis” covers sepsis that occurs as the result of pregnancy, delivery, or infection during the post-partum period. But there are other terms that may be used as well, such as puerperal fever, puerperal sepsis, and post-partum sepsis.
Reducing the incidence of maternal sepsis
Sepsis can’t always be prevented, but the risk can be reduced significantly by taking certain steps to prevent or quickly treat infections. Here are some suggestions:
- Be up-to-date on routine vaccinations
- If your doctor recommends an invasive procedure, ask why it is necessary and if there are any non-invasive options
- Reduce the number of vaginal examinations during labor
- Ask anyone who touches you if they have washed their hands first
- Contact your healthcare provider if your membranes rupture prematurely
- If a Cesarean section is recommended, ask why and if there is an option for a vaginal birth when possible
- Following childbirth, report if you experience a fever, any increase of abdominal pain or bleeding, or any foul smelling vaginal discharge
- Contact your healthcare provider if you suspect you have an infection
- After childbirth, follow your provider’s instructions regarding care of your vaginal area or your surgical incision
There are over 50 submissions about women who had maternal sepsis in the Faces of Sepsis collection of stories. Some were written by women who survived, while others were submitted by loved ones who were left behind.
Having a baby can turn your whole world sideways, but by being aware of maternal sepsis, you can reduce your risk of adding to the stress by becoming ill.
1- Maternal mortality and morbidity in the United States of America. World Health Organization. March 2015. http://www.who.int/bulletin/volumes/93/3/14-148627/en/
2- Pregnancy Mortality Surveillance System. Centers for Disease Control and Prevention. Accessed April 20, 2018. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html
3- Sepsis Standard Work: Improving Compliance with Early Recognition and Management of Perinatal Sepsis. Centers for Disease Control and Prevention. May 17, 2017. https://www.cdc.gov/infectioncontrol/pdf/webinarslides/CDC-ANA-AWHONN-SCCM-Maternal-Sepsis-Webinar_1.pdf
4- Sepsis and Pregnancy & Childbirth. Sepsis Alliance. December 14, 2017. https://www.sepsis.org/sepsis-and/pregnancy-and-childbirth/





























